Down syndrome
| Down syndrome | |
|---|---|
| Classification and external resources | |
 Boy with Down syndrome assembling a bookcase |
|
| ICD-10 | Q90. |
| ICD-9 | 758.0 |
| OMIM | 190685 |
| DiseasesDB | 3898 |
| MedlinePlus | 000997 |
| eMedicine | ped/615 |
| MeSH | D004314 |
| Disability |
|---|
 |
| Disability in practice |
| Disability Theory · Ableism/Disablism Society for Disability Studies |
| Disabled sports |
| Special Olympics · Paralympics Deaflympics · Extremity Games |
| Societal implications |
| Disability rights People-first language |
| Structural and Assistive |
| Personal Care Assistant Activities of Daily Living |
| Socioeconomic assistance |
| SSDI · SSI · DLA · ODSP Students · Rail |
| Disability activist groups |
| DPI · Visitability |
| Inclusive arts and media |
| Disability in the arts Disability in the media |
| Portal (categories · lists) |
Down syndrome, or Down's syndrome (primarily in the United Kingdom),[1][2] trisomy 21, or trisomy G, is a chromosomal disorder caused by the presence of all or part of an extra 21st chromosome. It is named after John Langdon Down, the British physician who described the syndrome in 1866. The disorder was identified as a chromosome 21 trisomy by Jérôme Lejeune in 1959. The condition is characterized by a combination of major and minor differences in structure. Often Down syndrome is associated with some impairment of cognitive ability and physical growth, and a particular set of facial characteristics. Down syndrome in a fetus can be identified with amniocentesis during pregnancy, or in a baby at birth.
Individuals with Down syndrome tend to have a lower-than-average cognitive ability, often ranging from mild to moderate disabilities. A small number have severe to profound mental disability. The average IQ of children with Down syndrome is around 50, compared to normal children with an IQ of 100.[3] The incidence of Down syndrome is estimated at 1 per 800 to 1,000 births, although it is statistically much more common with older mothers. Other factors may also play a role.
Many of the common physical features of Down syndrome may also appear in people with a standard set of chromosomes, including microgenia (an abnormally small chin),[4] an unusually round face, macroglossia[5] (protruding or oversized tongue), an almond shape to the eyes caused by an epicanthic fold of the eyelid, upslanting palpebral fissures (the separation between the upper and lower eyelids), shorter limbs, a single transverse palmar crease (a single instead of a double crease across one or both palms, also called the Simian crease), poor muscle tone, and a larger than normal space between the big and second toes. Health concerns for individuals with Down syndrome include a higher risk for congenital heart defects, gastroesophageal reflux disease, recurrent ear infections, obstructive sleep apnea, and thyroid dysfunctions.
Early childhood intervention, screening for common problems, medical treatment where indicated, a conducive family environment, and vocational training can improve the overall development of children with Down syndrome. Although some of the physical genetic limitations of Down syndrome cannot be overcome, education and proper care will improve quality of life.[6]
Contents |
Signs and symptoms
Down syndrome can result from several different genetic mechanisms. This results in a wide variability in individual signs and symptoms due to complex gene and environment interactions. Prior to birth, it is not possible to predict the symptoms that an individual with Down syndrome will develop.
Individuals with Down syndrome may have some or all of the following physical characteristics: microgenia (abnormally small chin),[4] oblique eye fissures with epicanthic skin folds on the inner corner of the eyes (formerly known as a mongoloid fold),[5] muscle hypotonia (poor muscle tone), a flat nasal bridge, a single palmar fold, a protruding tongue (due to small oral cavity, and an enlarged tongue near the tonsils) or macroglossia,[5] a short neck, white spots on the iris known as Brushfield spots,[7] excessive joint laxity including atlanto-axial instability, excessive space between large toe and second toe, a single flexion furrow of the fifth finger, and a higher number of ulnar loop dermatoglyphs. Most individuals with Down syndrome have mental retardation in the mild (IQ 50–70) to moderate (IQ 35–50) range,[8] with individuals having Mosaic Down syndrome typically 10–30 points higher.[9] They also may have a broad head and a very round face.
Language skills show a difference between understanding speech and expressing speech, and commonly individuals with Down syndrome have a speech delay.[10] Fine motor skills are delayed[11] and often lag behind gross motor skills and can interfere with cognitive development. Effects of the disorder on the development of gross motor skills are quite variable. Some children will begin walking at around 2 years of age, while others will not walk until age 4. Physical therapy, and/or participation in a program of adapted physical education (APE), may promote enhanced development of gross motor skills in Down syndrome children.[12]
Growth parameters such as height, weight, and head circumference are smaller in children with DS than with normal individuals of the same age. Adults with DS tend to have short stature — the average height for men is 5 feet 1 inch (157 cm) and for women is four feet 9 inches (144 cm).[13] Individuals with DS are also at increased risk for obesity as they age.[14]
Complications
Individuals with Down syndrome have a higher risk for many conditions. The medical consequences of the extra genetic material in Down syndrome are highly variable and may affect the function of any organ system or bodily process. Some problems are present at birth, such as certain heart malformations. Others become apparent over time, such as epilepsy.
Congenital heart disease
The incidence of congenital heart disease in children with Down syndrome is up to 50%.[15] A ventricular septal defect is the most common form.
Malignancies
Hematologic malignancies such as leukemia are more common in children with DS. In particular, the risk for acute lymphoblastic leukemia is at least 10 times more common in DS and for the megakaryoblastic form of acute myelogenous leukemia is at least 50 times more common in DS. Transient leukemia is a form of leukemia which is rare in individuals without DS but affects up to 20 percent of newborns with DS. This form of leukemia is typically benign and resolves on its own over several months, though it can lead to other serious illnesses.[16] In contrast to hematologic malignancies, solid tumor malignancies are less common in DS, possibly due to increased numbers of tumor suppressor genes contained in the extra genetic material.[17]
Thyroid disorders
Individuals with DS are at increased risk for dysfunction of the thyroid gland, an organ which helps control metabolism. Low thyroid (hypothyroidism) is most common, occurring in almost a third of those with DS. This can be due to absence of the thyroid at birth (congenital hypothyroidism) or due to attack on the thyroid by the immune system.[18] Reproduction is also affected by DS.
Gastrointestinal
Down syndrome increases the risk of Hirschsprung's disease, in which the nerve cells that control the function of parts of the colon are not present.[19] This results in severe constipation. Other congenital anomalies occurring more frequently in DS include duodenal atresia, annular pancreas, and imperforate anus. Gastroesophageal reflux disease and celiac disease are also more common among people with DS.[20]
Infertility
There is infertility amongst both males and females with Down syndrome; males are usually unable to father children, while females demonstrate significantly lower rates of conception relative to unaffected individuals. Women with DS are less fertile and often have difficulties with miscarriage, premature birth, and difficult labor. Without preimplantation genetic diagnosis, approximately half of the offspring of someone with Down syndrome also have the syndrome themselves.[21] Men with DS are almost uniformly infertile, exhibiting defects in spermatogenesis.[22] There have been only three recorded instances of males with Down syndrome fathering children.[23][24]
Neurology
Children and adults with DS are at increased risk for developing epilepsy.[25][26] The risk for Alzheimer's disease is increased in individuals with DS, with 10-25% of individuals with DS showing signs of AD before age 50, up to 50% with clinical symptoms in the sixth decade, and up to 75% in the 7th decade. This sharp increase in the incidence and prevalence of dementia may be one of the factors driving the decreased life expectancy of persons with Down Syndrome.
Ophthalmology and otolaryngology
Eye disorders are more common in people with DS. Almost half have strabismus, in which the two eyes do not move in tandem. Refractive errors requiring glasses or contacts are also common. Cataracts (opacity of the lens) and glaucoma (increased eye pressures) are also more common in DS.[27] Brushfield spots (small white or grayish/brown spots on the periphery of the iris) may be present.
Other complications
In the past, prior to current treatment, there was a 38-78% incidence of hearing loss in children with Down syndrome. Fortunately, with aggressive, meticulous and compulsive diagnosis and treatment of chronic ear disease (e.g. otitis media, also known as Glue-ear) in children with Down syndrome, approximately 98% of the children have normal hearing levels. [28]
Instability of the atlanto-axial joint occurs in ~15% of people with DS, probably due to ligamental laxity. It may lead to the neurologic symptoms of spinal cord compression.[29] Periodic screening, with cervical x-rays, is recommended to identify this abnormality.
Other serious illnesses include immune deficiencies.
Decreased incidence of many cancer types
However, health benefits of Down syndrome include greatly reduced incidence of many common malignancies except leukemia and testicular cancer[30] — although it is, as yet, unclear whether the reduced incidence of various fatal cancers among people with Down syndrome is as a direct result of tumor-suppressor genes on chromosome 21,[31] because of reduced exposure to environmental factors that contribute to cancer risk, or some other as-yet unspecified factor. In addition to a reduced risk of most kinds of cancer, people with Down syndrome also have a much lower risk of hardening of the arteries and diabetic retinopathy.[32]
Genetics

Down syndrome is a chromosomal abnormality characterized by the presence of an extra copy of genetic material on the 21st chromosome, either in whole (trisomy 21) or part (such as due to translocations). The effects of the extra copy vary greatly among people, depending on the extent of the extra copy, genetic history, and pure chance. Down syndrome occurs in all human populations, and analogous effects have been found in other species such as chimpanzees[33] and mice. Recently, researchers have created transgenic mice with most of human chromosome 21 (in addition to the normal mouse chromosomes).[34] The extra chromosomal material can come about in several distinct ways. A typical human karyotype is designated as 46,XX or 46,XY, indicating 46 chromosomes with an XX arrangement typical of females and 46 chromosomes with an XY arrangement typical of males.[35]
Trisomy 21
Trisomy 21 (47,XX,+21) is caused by a meiotic nondisjunction event. With nondisjunction, a gamete (i.e., a sperm or egg cell) is produced with an extra copy of chromosome 21; the gamete thus has 24 chromosomes. When combined with a normal gamete from the other parent, the embryo now has 47 chromosomes, with three copies of chromosome 21. Trisomy 21 is the cause of approximately 95% of observed Down syndromes, with 88% coming from nondisjunction in the maternal gamete and 8% coming from nondisjunction in the paternal gamete.[36]
Mosaicism
Trisomy 21 is usually caused by nondisjunction in the gametes prior to conception, and all cells in the body are affected. However, when some of the cells in the body are normal and other cells have trisomy 21, it is called mosaic Down syndrome (46,XX/47,XX,+21).[37][38] This can occur in one of two ways: a nondisjunction event during an early cell division in a normal embryo leads to a fraction of the cells with trisomy 21; or a Down syndrome embryo undergoes nondisjunction and some of the cells in the embryo revert to the normal chromosomal arrangement. There is considerable variability in the fraction of trisomy 21, both as a whole and among tissues. This is the cause of 1–2% of the observed Down syndromes.[36]
Robertsonian translocation
The extra chromosome 21 material that causes Down syndrome may be due to a Robertsonian translocation in the karyotype of one of the parents. In this case, the long arm of chromosome 21 is attached to another chromosome, often chromosome 14 [45,XX,der(14;21)(q10;q10)]. A person with such a translocation is phenotypically normal. During reproduction, normal disjunctions leading to gametes have a significant chance of creating a gamete with an extra chromosome 21, producing a child with Down syndrome. Translocation Down syndrome is often referred to as familial Down syndrome. It is the cause of 2–3% of observed cases of Down syndrome.[36] It does not show the maternal age effect, and is just as likely to have come from fathers as mothers.
Duplication of a portion of chromosome 21
Rarely, a region of chromosome 21 will undergo a duplication event. This will lead to extra copies of some, but not all, of the genes on chromosome 21 (46,XX, dup(21q)).[39] If the duplicated region has genes that are responsible for Down syndrome physical and mental characteristics, such individuals will show those characteristics. This cause is rare and no rate estimates are available.
Screening
Pregnant women can be screened for various complications during pregnancy. Many standard prenatal screens can discover Down syndrome. Genetic counseling along with genetic testing, such as amniocentesis, chorionic villus sampling (CVS), or percutaneous umbilical cord blood sampling (PUBS) are usually offered to families who may have an increased chance of having a child with Down syndrome, or where normal prenatal exams indicate possible problems. In the United States, ACOG guidelines recommend that non-invasive screening and invasive testing be offered to all women, regardless of their age, and most likely all physicians currently follow these guidelines. However, some insurance plans will only reimburse invasive testing if a woman is >34 years old or if she has received a high-risk score from a non-invasive screening test.
Amniocentesis and CVS are considered invasive procedures, in that they involve inserting instruments into the uterus, and therefore carry a small risk of causing fetal injury or miscarriage. The risks of miscarriage for CVS and amniocentesis are often quoted as 1% and 0.5% respectively. There are several common non-invasive screens that can indicate a fetus with Down syndrome. These are normally performed in the late first trimester or early second trimester. Due to the nature of screens, each has a significant chance of a false positive, suggesting a fetus with Down syndrome when, in fact, the fetus does not have this genetic abnormality. Screen positives must be verified before a Down syndrome diagnosis is made. Common screening procedures for Down syndrome are given in Table 1.
| Screen | When performed (weeks gestation) | Detection rate | False positive rate | Description |
|---|---|---|---|---|
| Quad screen | 15–20 | 81%[32] | 5% | This test measures the maternal serum alpha feto protein (a fetal liver protein), estriol (a pregnancy hormone), human chorionic gonadotropin (hCG, a pregnancy hormone), and inhibin-Alpha (INHA).[40] |
| Nuchal translucency/free beta/PAPPA screen (aka "1st Trimester Combined Test") | 10–13.5 | 85%[41] | 5% | Uses ultrasound to measure Nuchal Translucency in addition to the freeBeta hCG and PAPPA (pregnancy-associated plasma protein A). NIH has confirmed that this first trimester test is more accurate than second trimester screening methods.[42] Performing an NT ultrasound requires considerable skill; a Combined test may be less accurate if there is operator error, resulting in a lower-than-advertised sensitivity and higher false-positive rate, possibly in the 5-10% range. |
| Integrated Test | 10-13.5 and 15–20 | 95%[43] | 5% | The Integrated test uses measurements from both the 1st Trimester Combined test and the 2nd trimester Quad test to yield a more accurate screening result. Because all of these tests are dependent on accurate calculation of the gestational age of the fetus, the real-world false-positive rate is >5% and maybe be closer to 7.5%. |
Even with the best non-invasive screens, the detection rate is 90%–95% and the rate of false positive is 2%–5%. Inaccuracies can be caused by undetected multiple fetuses (very rare with the ultrasound tests), incorrect date of pregnancy, or normal variation in the proteins. Because of the low base rate of Down Syndrome in young mothers, first- and second-trimester screens are much less useful for younger pregnant women; a positive screening test for a forty-year-old reveals around a 40% risk that the fetus has Down Syndrome; but for a twenty-year-old, a positive test means only a 2% chance that the fetus has Down syndrome. Thus younger women are rarely tested.
Confirmation of screen positive is normally accomplished with amniocentesis or chorionic villus sampling (CVS). Amniocentesis is an invasive procedure and involves taking amniotic fluid from the amniotic sac and identifying fetal cells. The lab work can take several weeks but will detect over 99.8% of all numerical chromosomal problems with a very low false positive rate.[44]
Ethical issues
A 2002 literature review of elective abortion rates found that 91–93% of pregnancies in the United Kingdom and Europe with a diagnosis of Down syndrome were terminated.[45] Data from the National Down Syndrome Cytogenetic Register in the United Kingdom indicates that from 1989 to 2006 the proportion of women choosing to terminate a pregnancy following prenatal diagnosis of Down Syndrome has remained constant at around 92%.[46][47] Some physicians and ethicists are concerned about the ethical ramifications of this.[48] Conservative commentator George Will called it "eugenics by abortion".[49] British peer Lord Rix stated that "alas, the birth of a child with Down's syndrome is still considered by many to be an utter tragedy" and that the "ghost of the biologist Sir Francis Galton, who founded the eugenics movement in 1885, still stalks the corridors of many a teaching hospital".[50] Doctor David Mortimer has argued in Ethics & Medicine that "Down's syndrome infants have long been disparaged by some doctors and government bean counters."[51] Some members of the disability rights movement "believe that public support for prenatal diagnosis and abortion based on disability contravenes the movement's basic philosophy and goals."[52]
Medical ethicist Ronald Green argues that parents have an obligation to avoid 'genetic harm' to their offspring,[53] and Claire Rayner, then a patron of the Down's Syndrome Association, defended testing and abortion saying "The hard facts are that it is costly in terms of human effort, compassion, energy, and finite resources such as money, to care for individuals with handicaps... People who are not yet parents should ask themselves if they have the right to inflict such burdens on others, however willing they are themselves to take their share of the burden in the beginning."[54] Peter Singer argued that "neither haemophilia nor Down's syndrome is so crippling as to make life not worth living, from the inner perspective of the person with the condition. To abort a fetus with one of these disabilities, intending to have another child who will not be disabled, is to treat fetuses as interchangeable or replaceable. If the mother has previously decided to have a certain number of children, say two, then what she is doing, in effect, is rejecting one potential child in favour of another. She could, in defence of her actions, say: the loss of life of the aborted fetus is outweighed by the gain of a better life for the normal child who will be conceived only if the disabled one dies."[55]
Management
Treatment of individuals with Down Syndrome depends on the particular manifestations of the disorder. For instance, individuals with congenital heart disease may need to undergo major corrective surgery soon after birth. Other individuals may have relatively minor health problems requiring no therapy.
Examination at birth
Initial examination of newborns with DS should pay particular attention to certain physical signs which are more commonly found in DS. Evaluation of the red reflex can help identify congenital cataracts. Movement of the eyes should be observed to identify strabismus. Constipation should raise concerns for Hirschsprung's disease and feeding problems should prompt intense education to ensure adequate input and nutrition.
At birth, an ultrasound of the heart (echocardiogram) should be done immediately in order to identify congenital heart disease (this should be carried out by someone with experience in pediatric cardiology). A complete blood count should be done in order to identify pre-existing leukemia. A hearing test using brainstem auditory evoked responses (BAERS) testing should be performed and any hearing deficits further characterized. The thyroid function should also be tested. Early Childhood Intervention should be involved from birth to help coordinate and plan effective strategies for learning and development.
The American Academy of Pediatrics, among other health organizations, has issued a series of recommendations for screening individuals with Down Syndrome for particular diseases.[56] These guidelines enable health care providers to identify and prevent important aspects of DS. All other typical newborn, childhood, and adult screening and vaccination programs should also be performed.
Plastic surgery
Plastic surgery has sometimes been advocated and performed on children with Down syndrome, based on the assumption that surgery can reduce the facial features associated with Down syndrome, therefore decreasing social stigma, and leading to a better quality of life.[57] Plastic surgery on children with Down syndrome is uncommon,[58] and continues to be controversial. Researchers have found that for facial reconstruction, "...although most patients reported improvements in their child's speech and appearance, independent raters could not readily discern improvement...."[59] For partial glossectomy (tongue reduction), one researcher found that 1 out of 3 patients "achieved oral competence," with 2 out of 3 showing speech improvement.[60] Len Leshin, physician and author of the ds-health website, has stated, "Despite being in use for over twenty years, there is still not a lot of solid evidence in favor of the use of plastic surgery in children with Down syndrome."[61] The National Down Syndrome Society has issued a "Position Statement on Cosmetic Surgery for Children with Down Syndrome"[62] which states that "The goal of inclusion and acceptance is mutual respect based on who we are as individuals, not how we look."
Cognitive development
The identification of the best methods of teaching each particular child ideally begins soon after birth through early intervention programs.[63] Cognitive development in children with Down syndrome is quite variable. It is not currently possible at birth to predict the capabilities of any individual reliably, nor are the number or appearance of physical features predictive of future ability. Since children with Down syndrome have a wide range of abilities, success at school can vary greatly, which underlines the importance of evaluating children individually. The cognitive problems that are found among children with Down syndrome can also be found among typical children. Therefore, parents can use general programs that are offered through the schools or other means.
Individuals with Down syndrome differ considerably in their language and communication skills. It is routine to screen for middle ear problems and hearing loss; low gain hearing aids or other amplification devices can be useful for language learning. Early communication intervention fosters linguistic skills. Language assessments can help profile strengths and weaknesses; for example, it is common for receptive language skills to exceed expressive skills. Individualized speech therapy can target specific speech errors, increase speech intelligibility, and in some cases encourage advanced language and literacy. Augmentative and alternative communication (AAC) methods, such as pointing, body language, objects, or graphics are often used to aid communication. Relatively little research has focused on the effectiveness of communications intervention strategies.[64]
In education, mainstreaming of children with Down syndrome is becoming less controversial in many countries. For example, there is a presumption of mainstream in many parts of the UK. Mainstreaming is the process whereby students of differing abilities are placed in classes with their chronological peers. Children with Down syndrome may not age emotionally/socially and intellectually at the same rates as children without Down syndrome, so over time the intellectual and emotional gap between children with and without Down syndrome may widen. Complex thinking as required in sciences but also in history, the arts, and other subjects can often be beyond the abilities of some, or achieved much later than in other children. Therefore, children with Down syndrome may benefit from mainstreaming provided that some adjustments are made to the curriculum.[65]
Some European countries such as Germany and Denmark advise a two-teacher system, whereby the second teacher takes over a group of children with disabilities within the class. A popular alternative is cooperation between special schools and mainstream schools. In cooperation, the core subjects are taught in separate classes, which neither slows down the typical students nor neglects the students with disabilities. Social activities, outings, and many sports and arts activities are performed together, as are all breaks and meals.[66]
Speech delay may require speech therapy to improve expressive language.[67]
Childhood and adulthood follow-up
As children with DS grow, their progress should be plotted on a growth chart in order to detect deviations from expected growth. Special growth charts are available so that children with DS can be compared with other children with DS. Thyroid function testing should be performed at 6 months and 12 months of age as well as yearly thereafter. Evaluation of the ears for infection as well as objective hearing tests should be performed at every visit. Formal evaluation for refractive errors requiring glasses should be performed at least every two years with subjective vision assessments with each visit. After the age of three, an x-ray of the neck should be obtained to screen for atlanto-axial instability. As the child ages, yearly symptom screening for obstructive sleep apnea should be performed.[56]
Alternative treatment
The Institutes for the Achievement of Human Potential is a non-profit organization which treats children who have, as the IAHP terms it, "some form of brain injury," including children with Down syndrome. The approach of "Psychomotor Patterning" is not proven,[68] and is considered alternative medicine.
Prognosis
These factors can contribute to a shorter life expectancy for people with Down syndrome. One study, carried out in the United States in 2002, showed an average lifespan of 49 years, with considerable variations between different ethnic and socio-economic groups.[69] However, in recent decades, the life expectancy among persons with Down syndrome has increased significantly up from 25 years in 1980. The causes of death have also changed, with chronic neurodegenerative diseases becoming more common as the population ages. Most people with Down Syndrome who survive into their 40s and 50s begin to suffer from an Alzheimer's disease-like dementia.[70]
Epidemiology
The incidence of Down syndrome is estimated at one per 800 to one per 1000 births.[71] In 2006, the Centers for Disease Control and Prevention estimated the rate as one per 733 live births in the United States (5429 new cases per year).[72] Approximately 95% of these are trisomy 21. Down syndrome occurs in all ethnic groups and among all economic classes.
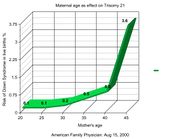
Maternal age influences the chances of conceiving a baby with Down syndrome. At maternal age 20 to 24, the probability is one in 1562; at age 35 to 39 the probability is one in 214, and above age 45 the probability is one in 19.[73] Although the probability increases with maternal age, 80% of children with Down syndrome are born to women under the age of 35,[74] reflecting the overall fertility of that age group. Recent data also suggest that paternal age, especially beyond 42,[75] also increases the risk of Down syndrome manifesting.[76]
Current research (as of 2008) has shown that Down syndrome is due to a random event during the formation of sex cells or pregnancy. There has been no evidence that it is due to parental behavior (other than age) or environmental factors.
History
English physician John Langdon Down first characterized Down syndrome as a distinct form of mental disability in 1862, and in a more widely published report in 1866.[77] Due to his perception that children with Down syndrome shared physical facial similarities (epicanthal folds) with those of Blumenbach's Mongolian race, Down used the term mongoloid, derived from prevailing ethnic theory.[78] Attitudes about Down syndrome were very much tied to racism and colonialism until as recently as the 1970s.
By the 20th century, Down syndrome had become the most recognizable form of mental disability. Most individuals with Down syndrome were institutionalized, few of the associated medical problems were treated, and most died in infancy or early adult life. With the rise of the eugenics movement, 33 of the (then) 48 U.S. states and several countries began programs of forced sterilization of individuals with Down syndrome and comparable degrees of disability. The ultimate expression of this type of public policy was "Action T4" in Nazi Germany, a program of systematic murder. Court challenges, scientific advances and public revulsion led to discontinuation or repeal of such sterilization programs during the decades after World War II.
Until the middle of the 20th century, the cause of Down syndrome remained unknown. However, the presence in all races, the association with older maternal age, and the rarity of recurrence had been noticed. Standard medical texts assumed it was caused by a combination of inheritable factors which had not been identified. Other theories focused on injuries sustained during birth.[79]
With the discovery of karyotype techniques in the 1950s, it became possible to identify abnormalities of chromosomal number or shape. In 1959, Jérôme Lejeune discovered that Down syndrome resulted from an extra chromosome.[80][81] The extra chromosome was subsequently labeled as the 21st, and the condition as trisomy 21.
In 1961, eighteen geneticists wrote to the editor of The Lancet suggesting that Mongolian idiocy had "misleading connotations," had become "an embarrassing term," and should be changed.[82] The Lancet supported Down's Syndrome. The World Health Organization (WHO) officially dropped references to mongolism in 1965 after a request by the Mongolian delegate.[83] However, almost 40 years later, the term ‘mongolism’ still appears in leading medical texts such as General and Systematic Pathology, 4th Edition, 2004, edited by Professor Sir James Underwood. Advocacy groups adapted and parents groups welcomed the elimination of the Mongoloid label that had been a burden to their children. The first parents group in the United States, the Mongoloid Development Council, changed its name to the National Association for Down Syndrome in 1972 [1].
In 1975, the United States National Institutes of Health convened a conference to standardize the nomenclature of malformations. They recommended eliminating the possessive form: "The possessive use of an eponym should be discontinued, since the author neither had nor owned the disorder."[84] Although both the possessive and non-possessive forms are used in the general population, Down syndrome is the accepted term among professionals in the USA, Canada and other countries; Down's syndrome is still used in the United Kingdom and other areas.[85]
Society and culture
Advocates for people with Down syndrome point to various factors, such as additional educational support and parental support groups to improve parenting knowledge and skills. There are also strides being made in education, housing, and social settings to create environments which are accessible and supportive to people with Down syndrome. In most developed countries, since the early twentieth century many people with Down syndrome were housed in institutions or colonies and excluded from society. However, since the early 1960s parents and their organizations, educators and other professionals have generally advocated a policy of inclusion,[86] bringing people with any form of mental or physical disability into general society as much as possible. Such organizations included the National Association for Down Syndrome, the first known organization advocating for Down Syndrome individuals in the United States founded by Kathryn McGee in 1960 [2]; MENCAP advocating for all with mental disabilities, which was founded in the U.K. in 1946 by Judy Fryd [3]; and the National Down Syndrome Congress, the first truly national organization in the U.S. advocating for Down Syndrome families, founded in 1973 by Kathryn McGee and others [4] Kathryn McGee. In many countries, people with Down syndrome are educated in the normal school system; there are increasingly higher-quality opportunities to move from special (segregated) education to regular education settings.
Despite these changes, the additional support needs of people with Down syndrome can still pose a challenge to parents and families. Although living with family is preferable to institutionalization, people with Down syndrome often encounter patronizing attitudes and discrimination in the wider community.
The first World Down Syndrome Day was held on 21 March 2006. The day and month were chosen to correspond with 21 and trisomy respectively. It was proclaimed by European Down Syndrome Association during their European congress in Palma de Mallorca (febr. 2005). In the United States, the National Down Syndrome Society observes Down Syndrome Month every October as "a forum for dispelling stereotypes, providing accurate information, and raising awareness of the potential of individuals with Down syndrome."[87] In South Africa, Down Syndrome Awareness Day is held every October 20.[88] Organizations such as Special Olympics Hawaii provide year-round sports training for individuals with intellectual disabilities such as Down syndrome.
Notable individuals
- Stephane Ginnsz, actor (Duo)—In 1996 was first actor with Down syndrome in the lead part of a motion picture.[89]
- Pascal Duquenne, Belgian film actor, co-starred with Daniel Auteuil in the 1996 film Le Huitième Jour (The Eighth Day), both actors won the joint award for Best Actor at the Cannes Film Festival.
- Joey Moss, Edmonton Oilers locker room attendant.[90]
- Isabella Pujols, adopted daughter of St. Louis Cardinals first baseman Albert Pujols and inspiration for the Pujols Family Foundation.[91]
- Trig Palin, son of Sarah Palin and her husband Todd.
- Paula Sage, Scottish film actress and Special Olympics netball athlete.[92] Her role in the 2003 film AfterLife brought her a BAFTA Scotland award for best first time performance and Best Actress in the Bratislava International Film Festival, 2004.[93]
- Chris Burke, American actor who portrayed "Corky Thatcher" on the television series Life Goes On and "Taylor" on Touched By An Angel.
- Edward Barbanell, played Billy in 2005's The Ringer.
- Danny Alsabbagh, Australian actor who played Toby in the Australian mockumentary series Summer Heights High
- Tommy Jessop, British actor who played Ben in Coming Down the Mountain, opposite Nicholas Hoult
- Rene Moreno, subject of "Up Syndrome" - a documentary film about life with Down syndrome.[94][95]
- Nigel Hunt, British author (The World Of Nigel Hunt; The Diary Of A Mongoloid Youth—this book was published in 1967, when "mongoloid" was still quite commonly used to refer to people with Down's Syndrome).
- Hilly, Sam, Lucy and Megan, 4 friends with Down's Syndrome who share a house in Brighton with their friend Lewis who has Williams Syndrome Their lives are followed in the internet documentary series "The Specials".[96]
- Pablo Pineda, Spanish actor who starred in the semi-autobiographical film Yo También.[97]
- Andrea Friedman: actress who portrayed Corky's girlfriend Amanda in Life Goes On and Ellen in the Family Guy episode "Extra Large Medium".[98]
Portrayal in fiction
- Bret Lott: Jewel
- Bernice Rubens: A Solitary Grief
- Paul M Belous & Robert Wolterstorff: Quantum Leap: Jimmy
- Emily Perl Kingsley: Welcome to Holland
- The Kingdom and its American counterpart, Kingdom Hospital
- Stephen King: Dreamcatcher
- Dean Koontz: The Bad Place
- Jeffrey Eugenides: The Virgin Suicides
- Theodore Sturgeon: More Than Human
- Janet Mitchell, character in EastEnders
- Kim Edwards: The Memory Keeper's Daughter
- June Rae Wood: The Man Who Loved Clowns
- Jaco van Dormael: Le huitième jour
- Mark Haddon: Coming Down the Mountain (BBC Radio play and BBC TV Drama)
- Theodore "T-Bag" Bagwell's mother: Prison Break
- Chris Burke as Charles "Corky" Thatcher in Life Goes On
- "Toby": Summer Heights High
- Emily Perl Kingsley: Kids Like These (TV Movie)
- Lauren Potter as Becky Jackson in Glee
Research
Down syndrome is “a developmental abnormality characterized by trisomy of human chromosome 21" (Nelson 619). The extra copy of chromosome-21 leads to an over expression of certain genes located on chromosome-21.
Research by Arron et al. shows that some of the phenotypes associated with Down syndrome can be related to the disregulation of transcription factors (596), and in particular, NFAT. NFAT is controlled in part by two proteins, DSCR1 and DYRK1A; these genes are located on chromosome-21 (Epstein 582). In people with Down syndrome, these proteins have 1.5 times greater concentration than normal (Arron et al. 597). The elevated levels of DSCR1 and DYRK1A keep NFAT primarily located in the cytoplasm rather than in the nucleus, preventing NFATc from activating the transcription of target genes and thus the production of certain proteins (Epstein 583).
This disregulation was discovered by testing in transgenic mice that had segments of their chromosomes duplicated to simulate a human chromosome-21 trisomy (Arron et al. 597). A test involving grip strength showed that the genetically modified mice had a significantly weaker grip, much like the characteristically poor muscle tone of an individual with Down syndrome (Arron et al. 596). The mice squeezed a probe with a paw and displayed a .2 newton weaker grip (Arron et al. 596). Down syndrome is also characterized by increased socialization. When modified and unmodified mice were observed for social interaction, the modified mice showed as much as 25% more interactions as compared to the unmodified mice (Arron et al. 596).
The genes that may be responsible for the phenotypes associated may be located proximal to 21q22.3. Testing by Olson et al. in transgenic mice show the duplicated genes presumed to cause the phenotypes are not enough to cause the exact features. While the mice had sections of multiple genes duplicated to approximate a human chromosome-21 triplication, they only showed slight craniofacial abnormalities (688-690). The transgenic mice were compared to mice that had no gene duplication by measuring distances on various points on their skeletal structure and comparing them to the normal mice (Olson et al. 687). The exact characteristics of Down syndrome were not observed, so more genes involved for Down Syndrome phenotypes have to be located elsewhere.
Reeves et al., using 250 clones of chromosome-21 and specific gene markers, were able to map the gene in mutated bacteria. The testing had 99.7% coverage of the gene with 99.9995% accuracy due to multiple redundancies in the mapping techniques. In the study 225 genes were identified (311-313).
The search for major genes that may be involved in Down syndrome symptoms is normally in the region 21q21–21q22.3. However, studies by Reeves et al. show that 41% of the genes on chromosome-21 have no functional purpose, and only 54% of functional genes have a known protein sequence. Functionality of genes was determined by a computer using exon prediction analysis (312). Exon sequence was obtained by the same procedures of the chromosome-21 mapping.
Research has led to an understanding that two genes located on chromosome-21, that code for proteins that control gene regulators, DSCR1 and DYRK1A can be responsible for some of the phenotypes associated with Down syndrome. DSCR1 and DYRK1A cannot be blamed outright for the symptoms; there are a lot of genes that have no known purpose. Much more research would be needed to produce any appropriate or ethically acceptable treatment options.
Recent use of transgenic mice to study specific genes in the Down syndrome critical region has yielded some results. APP[99] is an Amyloid beta A4 precursor protein. It is suspected to have a major role in cognitive difficulties.[100] Another gene, ETS2[101] is Avian Erythroblastosis Virus E26 Oncogene Homolog 2. Researchers have "demonstrated that over-expression of ETS2 results in apoptosis. Transgenic mice over-expressing ETS2 developed a smaller thymus and lymphocyte abnormalities, similar to features observed in Down syndrome."[101]
Human chromosome 21 contains five microRNA genes: miR-99a, let-7c, miR-125b-2, miR-155,and miR-802. MiR-155 and miR-802 regulate the expression of the methyl-CpG-binding protein (MeCP2). It has been suggested that the underexpression of MeCP2, secondary to trisomic overexpression of Human chromosome 21 derived miRNAs, may result in aberrant expression of the transcription factors of CREB1 and MEF2C . This in turn may lead to abnormal brain development through anomalous neuronal gene expression during the critical period of synaptic maturation by alterating neurogenesis, neuronal differentiation, myelination, and synaptogenesis.[102]
Vitamin supplements, in particular supplemental antioxidants and folinic acid, have been shown to be ineffective in the treatment of Down syndrome.[103]
Footnotes
- ↑ DNA India
- ↑ Canadian Down Syndrome Society
- ↑ Liptak, Gregory S. (December 2008). "Down Syndrome (Trisomy 21; Trisomy G)". Merck Manual. http://www.merck.com/mmhe/sec23/ch266/ch266b.html#sec23-ch266-ch266b-420. Retrieved 2010-07-30. "Symptoms"
- ↑ 4.0 4.1 Meira Weiss (1994-02). Conditional love: parents' attitudes toward handicapped children. p. 94. ISBN 9780897893244. http://books.google.com/?id=a62J5GPHd3cC&pg=PA94&lpg=PA94&dq=%22down%27s+syndrome%22+chin+face. Retrieved 2009-07-22.
- ↑ 5.0 5.1 5.2 This discussion by Myron Belfer, M.D., book by Gottfried Lemperie, M.D., and Dorin Radu, M.D. (1980). "Facial Plastic Surgery in Children with Down's Syndrome (preview page, with link to full content on plasreconsurg.com)". p. 343. http://scholar.google.com/scholar?q=info:Nt6asksVAiYJ:scholar.google.com/&hl=en&output=viewport. Retrieved 2009-07-22.
- ↑ Roizen NJ, Patterson D (April 2003). "Down's syndrome" (Review). Lancet 361 (9365): 1281–9. doi:10.1016/S0140-6736(03)12987-X. PMID 12699967.
- ↑ "Definition of Brushfield's Spots". http://www.medterms.com/script/main/art.asp?articlekey=6570.
- ↑ American Academy of Pediatrics Committee on Genetics (February 2001). "American Academy of Pediatrics: Health supervision for children with Down syndrome". Pediatrics 107 (2): 442–449. doi:10.1542/peds.107.2.442. PMID 11158488.
- ↑ Strom, C. "FAQ from Mosaic Down Syndrome Society". http://www.mosaicdownsyndrome.com/faqs.htm. Retrieved 2006-06-03.
- ↑ Bird, G. and S. Thomas (2002). "Providing effective speech and language therapy for children with Down syndrome in mainstream settings: A case example". Down Syndrome News and Update 2 (1): 30–31. Also, Kumin, Libby (1998). "Comprehensive speech and language treatment for infants, toddlers, and children with Down syndrome". In Hassold, T.J.and D. Patterson. Down Syndrome: A Promising Future, Together. New York: Wiley-Liss.
- ↑ "Development of Fine Motor Skills in Down Syndrome". http://www.about-down-syndrome.com/fine-motor-skills-in-down-syndrome.html. Retrieved 2006-07-03.
- ↑ M. Bruni. "Occupational Therapy and the Child with Down Syndrome". http://www.ds-health.com/occther.htm. Retrieved 2006-06-02.
- ↑ Cronk C, Crocker AC, Pueschel SM, Shea AM, Zackai E, Pickens G, Reed RB.Growth charts for children with Down syndrome: 1 month to 18 years of age. Pediatrics. 1988 Jan;81(1):102-10. PMID 2962062
- ↑ Rubin SS, Rimmer JH, Chicoine B, Braddock D, McGuire DE. Overweight prevalence in persons with Down syndrome. Ment Retard. 1998 Jun;36(3):175-81. PMID 9638037
- ↑ [Cincinnati Children's Heart Institute > Heart-Related Syndromes - Down Syndrome (Trisomy 21)] Revised 8/09
- ↑ Transient leukaemia--a benign form of leukaemia in newborn infants with trisomy 21. Br J Haematol. 2003 Mar;120(6):930-8. Review. PMID 12648061
- ↑ Hasle H, Clemmensen IH, Mikkelsen M. Risks of leukaemia and solid tumours in individuals with Down's syndrome. Lancet. 2000 Jan 15;355(9199):165-9. PMID 10675114
- ↑ Karlsson B, Gustafsson J, Hedov G, Ivarsson SA, Anneren G. Thyroid dysfunction in Down's syndrome: relation to age and thyroid autoimmunity. Arch Dis Child. 1998 Sep;79(3):242-5. PMID 9875020
- ↑ Ikeda K, Goto S. Additional anomalies in Hirschsprung's disease: an analysis based on the nationwide survey in Japan. Z Kinderchir. 1986 Oct;41(5):279-81. PMID 2947399
- ↑ Zachor DA, Mroczek-Musulman E, Brown P. Prevalence of celiac disease in Down syndrome in the United States. J Pediatr Gastroenterol Nutr. 2000 Sep;31(3):275-9. PMID 10997372
- ↑ Hsiang YH, Berkovitz GD, Bland GL, Migeon CJ, Warren AC (1987). "Gonadal function in patients with Down syndrome". Am. J. Med. Genet. 27 (2): 449–58. doi:10.1002/ajmg.1320270223. PMID 2955699.
- ↑ Johannisson R, Gropp A, Winking H, Coerdt W, Rehder H, Schwinger E. Down's syndrome in the male. Reproductive pathology and meiotic studies. Hum Genet. 1983;63(2):132-8. PMID 6220959
- ↑ Sheridan R, Llerena J, Matkins S, Debenham P, Cawood A, Bobrow M (1989). "Fertility in a male with trisomy 21". J Med Genet 26 (5): 294–8. doi:10.1136/jmg.26.5.294. PMID 2567354.
- ↑ Pradhan M, Dalal A, Khan F, Agrawal S (2006). "Fertility in men with Down syndrome: a case report". Fertil Steril 86 (6): 1765.e1–3. doi:10.1016/j.fertnstert.2006.03.071. PMID 17094988.
- ↑ Goldberg-Stern H, Strawsburg RH, Patterson B, Hickey F, Bare M, Gadoth N, Degrauw TJ.Seizure frequency and characteristics in children with Down syndrome. Brain Dev. 2001 Oct;23(6):375-8. PMID 11578846
- ↑ Menendez M. Down syndrome, Alzheimer's disease and seizures. Brain Dev. 2005 Jun;27(4):246-52. Review. PMID 15862185
- ↑ Caputo AR, Wagner RS, Reynolds DR, Guo SQ, Goel AK. Down syndrome. Clinical review of ocular features. Clin Pediatr (Phila). 1989 Aug;28(8):355-8. PMID 2527102
- ↑ Shott SR, Joseph A, Heithaus D (December 2001). "Hearing loss in children with Down syndrome". Int. J. Pediatr. Otorhinolaryngol. 61 (3): 199–205. doi:10.1016/S0165-5876(01)00572-9. PMID 11700189.
- ↑ Pueschel SM, Scola FH. Atlantoaxial instability in individuals with Down syndrome: epidemiologic, radiographic, and clinical studies. Pediatrics. 1987 Oct;80(4):555-60. PMID 2958770
- ↑ Yang Q, Rasmussen SA, Friedman JM (March 2002). "Mortality associated with Down's syndrome in the USA from 1983 to 1997: a population-based study". Lancet 359 (9311): 1019–25. doi:10.1016/S0140-6736(02)08092-3. PMID 11937181. http://www.ds-health.com/abst/a0205.htm.
- ↑ Lee; Park, TI; Park, SH; Park, JY (2003). "Loss of heterozygosity on the long arm of chromosome 21 in non–small cell lung cancer". Ann Thorac Surg 75 (5): 1597–1600. doi:10.1016/S0003-4975(02)04902-0. PMID 12735585. http://ats.ctsnetjournals.org/cgi/content/full/75/5/1597.
- ↑ 32.0 32.1 ACOG Guidelines Bulletin #77 clearly state that the sensitivity of the Quad Test is 81%
- ↑ McClure HM, Belden KH, Pieper WA, Jacobson CB (September 1969). "Autosomal trisomy in a chimpanzee: resemblance to Down's syndrome". Science 165 (897): 1010–2. doi:10.1126/science.165.3897.1010. PMID 4240970.
- ↑ "Down's syndrome recreated in mice". BBC News. 2005-09-22. http://news.bbc.co.uk/1/hi/health/4268226.stm. Retrieved 2006-06-14.
- ↑ For a description of human karyotype see Mittleman, A. (editor) (1995). "An International System for Human Cytogenetic Nomeclature". http://www.iscn1995.org/. Retrieved 2006-06-04.
- ↑ 36.0 36.1 36.2 "Down syndrome occurrence rates (NIH)". http://www.nichd.nih.gov/publications/pubs/downsyndrome.cfm#TheOccurrence. Retrieved 2006-06-02.
- ↑ Mosaic Down syndrome on the Web.
- ↑ International Mosaic Down syndrome Association.
- ↑ Petersen MB, Tranebjaerg L, McCormick MK, Michelsen N, Mikkelsen M, Antonarakis SE (1990). "Clinical, cytogenetic, and molecular genetic characterization of two unrelated patients with different duplications of 21q". Am J Med Genet Suppl 7: 104–9. PMID 2149934.
- ↑ For a current estimate of rates, see Benn PA, Ying J, Beazoglou T, Egan JF (January 2001). "Estimates for the sensitivity and false-positive rates for second trimester serum screening for Down syndrome and trisomy 18 with adjustment for cross-identification and double-positive results". Prenat. Diagn. 21 (1): 46–51. doi:10.1002/1097-0223(200101)21:1<46::AID-PD984>3.0.CO;2-C. PMID 11180240.
- ↑ ACOG Guidelines Bulletin #77 state that the sensitivity of the Combined Test is 82-87%
- ↑ NIH FASTER study (NEJM 2005 (353):2001). See also J.L. Simplson's editorial (NEJM 2005 (353):19).
- ↑ ACOG Guidelines Bulletin #77 state that the sensitivity of the Integrated Test is 94-96%
- ↑ Fackler, A. "Down syndrome". http://health.yahoo.com/topic/children/baby/article/healthwise/hw167989. Retrieved 2006-09-07.
- ↑ Caroline Mansfield, Suellen Hopfer, Theresa M. Marteau (1999). "Termination rates after prenatal diagnosis of Down syndrome, spina bifida, anencephaly, and Turner and Klinefelter syndromes: a systematic literature review". Prenatal Diagnosis 19 (9): 808–812. doi:10.1002/(SICI)1097-0223(199909)19:9<808::AID-PD637>3.0.CO;2-B. PMID 10521836. http://www3.interscience.wiley.com/cgi-bin/abstract/65500197/ABSTRACT. This is similar to 90% results found by David W. Britt, Samantha T. Risinger, Virginia Miller, Mary K. Mans, Eric L. Krivchenia, Mark I. Evans (1999). "Determinants of parental decisions after the prenatal diagnosis of Down syndrome: Bringing in context". American Journal of Medical Genetics 93 (5): 410–416. doi:10.1002/1096-8628(20000828)93:5<410::AID-AJMG12>3.0.CO;2-F. PMID 10951466.
- ↑ "Society 'more positive on Down's'". BBC News. 2008-11-24. http://news.bbc.co.uk/1/hi/health/7746747.stm.
- ↑ Peter Horrocks (2008-12-05). "Changing attitudes?". BBC News. http://www.bbc.co.uk/blogs/theeditors/2008/12/changing_attitudes.html.
- ↑ Glover, NM and Glover, SJ (1996). "Ethical and legal issues regarding selective abortion of fetuses with Down syndrome". Ment. Retard. 34 (4): 207–214. PMID 8828339.
- ↑ Will, George (2005-04-01). "Eugenics By Abortion: Is perfection an entitlement?". Washington Post: A37. http://www.washingtonpost.com/wp-dyn/articles/A51671-2005Apr13.html.
- ↑ "Letter: Ghost of eugenics stalks Down's babies". http://findarticles.com/p/articles/mi_qn4158/is_20060524/ai_n16410413.
- ↑ "New Eugenics and the newborn: The historical "cousinage" of eugenics and infanticide, The". Ethics & Medicine. 2003. http://findarticles.com/p/articles/mi_qa4004/is_200310/ai_n9330668/pg_7.
- ↑ Erik Parens and Adrienne Asch (2003). "Disability rights critique of prenatal genetic testing: Reflections and recommendations". Mental Retardation and Developmental Disabilities Research Reviews 9 (1): 40–47. doi:10.1002/mrdd.10056. PMID 12587137. http://www3.interscience.wiley.com/cgi-bin/abstract/102531130/ABSTRACT. Retrieved 2006-07-03.
- ↑ Green, RM (1997). "Parental autonomy and the obligation not to harm one's child genetically". J Law Med Ethics 25 (1): 5–15. doi:10.1111/j.1748-720X.1997.tb01389.x. PMID 11066476.
- ↑ Rayner, Clare (27 June 1995). "ANOTHER VIEW: A duty to choose unselfishly". The Independent (London). http://www.independent.co.uk/opinion/another-view-a-duty-to-choose-unselfishly-1588540.html. Retrieved 2009-10-30.
- ↑ Singer, Peter (1993). "Taking Life: Humans". Practical ethics (2nd ed.). Cambridge University Press. pp. 395. ISBN 052143971X.
- ↑ 56.0 56.1 American Academy of Pediatrics Committee on Genetics. (2001) Health Supervision for Children With Down Syndrome. Pediatrics 107(2):442-449. Online at Health Supervision for Children With Down Syndrome. Accessed 13 August 2006
- ↑ Olbrisch RR (1982). "Plastic surgical management of children with Down syndrome: indications and results". British Journal of Plastic Surgery 35 (2): 195–200. doi:10.1016/0007-1226(82)90163-1. PMID 6211206.
- ↑ Parens, E. (editor) (2006). Surgically Shaping Children : Technology, Ethics, and the Pursuit of Normality. Baltimore: Johns Hopkins University Press. ISBN 0-8018-8305-9.
- ↑ Klaiman, P and E Arndt (1989). "Facial reconstruction in Down syndrome: perceptions of the results by parents and normal adolescents". Cleft Palate Journal 26 (3): 186–190; discussion 190–192. PMID 2527096. Also, see Arndt, EM, A Lefebvre, F Travis, and IR Munro (1986). "Fact and fantasy: psychosocial consequences of facial surgery in 24 Down syndrome children". Br J Plast Surg 4 (4): 498–504. doi:10.1016/0007-1226(86)90120-7. PMID 2946342.
- ↑ SA Pensler; Pensler, JM (1990). "The efficacy of tongue resection in treatment of symptomatic macroglossia in the child". Ann Plast Surg 25 (1): 14–17. doi:10.1097/00000637-199007000-00003. PMID 2143060.See also KM Van Lierde, H Vermeersch, J Van Borsel, P Van Cauwenberge (2002/2003). "The impact of a partial glossectomy on articulation and speech intelligibility". Oto-Rhino-Laryngologia Nova 12: 305–310. doi:10.1159/000083122.
- ↑ Leshin, L (2000). "Plastic Surgery in Children with Down Syndrome". http://www.ds-health.com/psurg.htm. Retrieved 2006-07-25.
- ↑ National Down Syndrome Society. "Position Statement on Cosmetic Surgery for Children with Down Syndrome". http://www.ndss.org/content.cfm?fuseaction=InfoRes.HlthArticle&article=34. Retrieved 2006-06-02.
- ↑ "Dear New or Expectant Parents". National Down Syndrome Society. http://www.ndss.org/index.php?option=com_content&task=view&id=2015&Itemid=198. Retrieved 2006-05-12. Also "Research projects - Early intervention and education". http://www.downsed.org/topics/early-intervention/. Retrieved 2006-06-02.
- ↑ Roberts JE, Price J, Malkin C (2007). "Language and communication development in Down syndrome". Ment Retard Dev Disabil Res Rev 13 (1): 26–35. doi:10.1002/mrdd.20136. PMID 17326116.
- ↑ S.E.Armstrong. "Inclusion: Educating Students with Down Syndrome with Their Non-Disabled Peers". http://www.altonweb.com/cs/downsyndrome/index.htm?page=ndssincl.html. Retrieved 2006-05-12. Also, see Debra L. Bosworth. "Benefits to Students with Down Syndrome in the Inclusion Classroom: K-3". http://www.altonweb.com/cs/downsyndrome/index.htm?page=bosworth.html. Retrieved 2006-06-12. Finally, see a survey by NDSS on inclusion, Gloria Wolpert (1996). "The Educational Challenges Inclusion Study". National Down Syndrome Society. http://www.altonweb.com/cs/downsyndrome/index.htm?page=wolpert.html. Retrieved 2006-06-28.
- ↑ There are many such programs. One is described by Action Alliance for Children, K. Flores. "Special needs, "mainstream" classroom". http://www.4children.org/news/103spec.htm. Retrieved 2006-05-13. Also, see Flores, K.. "Special needs, "mainstream" classroom". http://www.4children.org/pdf/103spec.pdf. Retrieved 2006-05-13.
- ↑ Bird, G. and S. Thomas (2002). "Providing effective speech and language therapy for children with Down syndrome in mainstream settings: A case example". Down Syndrome News and Update 2 (1): 30–31. Also, Kumin, Libby (1998). "Comprehensive speech and language treatment for infants, toddlers, and children with Down syndrome". In Hassold, T.J.and D. Patterson. Down Syndrome: A Promising Future, Together. New York: Wiley-Liss.
- ↑ For criticism of the method, see Novella, S. "Psychomotor Patterning". http://www.quackwatch.org/01QuackeryRelatedTopics/patterning.html. Retrieved 2006-06-02.
- ↑ Young, Emma (2002-03-22). "Down's syndrome lifespan doubles". New Scientist. http://www.newscientist.com/article.ns?id=dn2073. Retrieved 2006-10-14.
- ↑ McPhee, J.; Tierney, Lawrence M.; Papadakis, Maxine A. (1999). Current medical diagnosis & treatment 1999. Norwalk, CT: Appleton & Lange. p. 1546. ISBN 0-8385-1550-9.
- ↑ Based on estimates by National Institute of Child Health & Human Development "Down syndrome rates". Archived from the original on 2006-09-01. http://web.archive.org/web/20060901004316/http://www.nichd.nih.gov/publications/pubs/downsyndrome/down.htm#Questions. Retrieved 2006-06-21.
- ↑ Center for Disease Control (6 January 2006). "Improved National Prevalence Estimates for 18 Selected Major Birth Defects, United States, 1999–2001". Morbidity and Mortality Weekly Report 54 (51 & 52): 1301–5. http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5451a2.htm.
- ↑ Huether, C.A.; Ivanovich, J; Goodwin, B S; Krivchenia, E L; Hertzberg, V S; Edmonds, L D; May, D S; Priest, J H (1998). "Maternal age specific risk rate estimates for Down syndrome among live births in whites and other races from Ohio and metropolitan Atlanta, 1970-1989". J Med Genet 35 (6): 482–490. doi:10.1136/jmg.35.6.482. PMID 9643290.
- ↑ Estimate from "National Down Syndrome Center". http://www.ndsccenter.org/resources/package3.php. Retrieved 2006-04-21.
- ↑ "Prevalence and Incidence of Down Syndrome". Diseases Center-Down Syndrome. Adviware Pty Ltd.. 2008-02-04. http://www.wrongdiagnosis.com/d/down_syndrome/prevalence.htm. Retrieved 2008-02-17. "incidence increases...especially when...the father is older than age 42"
- ↑ Warner, Jennifer. "Dad's Age Raises Down Syndrome Risk, Too", "WebMD Medical News". http://www.webmd.com/infertility-and-reproduction/news/20030701/dad-age-down-syndrome. Retrieved 2007-09-29.
- ↑ Down, J.L.H. (1866). "Observations on an ethnic classification of idiots". Clinical Lecture Reports, London Hospital 3: 259–262. http://www.neonatology.org/classics/down.html. Retrieved 2006-07-14. For a history of the disorder, see OC Ward (1998). John Langdon Down, 1828–1896. Royal Society of Medicine Press. ISBN 1-85315-374-5. or Conor, Ward. "John Langdon Down and Down's syndrome (1828–1896)". http://www.intellectualdisability.info/values/history_DS.htm. Retrieved 2006-06-02.
- ↑ Conor, W.O. (1999). "John Langdon Down: The Man and the Message". Down Syndrome Research and Practice 6 (1): 19–24. doi:10.3104/perspectives.94.
- ↑ Warkany, J. (1971). Congenital Malformations. Chicago: Year Book Medical Publishers, Inc. pp. 313–314. ISBN 0-8151-9098-0.
- ↑ Lejeune J, Gautier M, Turpin R (1959). "Etude des chromosomes somatiques de neuf enfants mongoliens". Comptes Rendus Hebd Seances Acad Sci 248 (11): 1721–2. http://gallica.bnf.fr/ark:/12148/bpt6k32002/f1759.chemindefer.
- ↑ "Jérôme Lejeune Foundation". http://www.fondationlejeune.org/eng/Content/Fondation/professeurlj.asp. Retrieved 2006-06-02.
- ↑ Gordon, Allen (1961). "Mongolism (Correspondence)". The Lancet 1 (7180): 775.
- ↑ Howard-Jones, Norman (1979). "On the diagnostic term "Down's disease"". Medical History 23 (1): 102–104. PMID 153994.
- ↑ A planning meeting was held on 20 March 1974, resulting in a letter to The Lancet."Classification and nomenclature of malformation (Discussion)". The Lancet 303 (7861): 798. 1974. doi:10.1016/S0140-6736(74)92858-X. PMID 4132724. The conference was held 10–11 February 1975, and reported to The Lancet shortly afterward."Classification and nomenclature of morphological defects (Discussion)". The Lancet 305 (7905): 513. 1975. doi:10.1016/S0140-6736(75)92847-0. PMID 46972.
- ↑ Leshin, Len (2003). "What's in a name". http://www.ds-health.com/name.htm. Retrieved 2006-05-12.
- ↑ Inclusion. National Down Syndrome Society. http://www.ndss.org/index.php?option=com_content&task=view&id=1941&Itemid=236. Retrieved 2006-05-21.
- ↑ National Down Syndrome Society
- ↑ Down Syndrome South Africa.
- ↑ Stephane Ginnsz. "Film Actor with Down Syndrome". ginnsz.com. http://www.stephane.ginnsz.com/. Retrieved 2006-12-08.
- ↑ Lomon, Chris (2003-02-28). "NHL Alumni RBC All-Star Awards Dinner". NHL Alumni. http://www.nhlalumni.com/slam/hockey/nhlalumni/news/03/0228.html. Retrieved 2006-12-08.
- ↑ "Pujols Family Foundation Home Page". http://www.pujolsfamilyfoundation.org/index2.html. Retrieved 2006-12-08.
- ↑ "Special Olympic Athlete Stars in Movie". http://www.specialolympics.org/Special+Olympics+Public+Website/English/Press_Room/Global_News_Archive/2004+Global+News+Archive/Special+Olympics+athlete+stars+in+movie.htm. Retrieved 2007-11-05.
- ↑ "Bratislava International Film festival 2004". http://www.imdb.com/Sections/Awards/Bratislava_International_Film_Festival/2004. Retrieved 2007-11-05.
- ↑ "Up Syndrome on the Internet Movie Database". http://us.imdb.com/title/tt0261375/. Retrieved 2009-04-19.
- ↑ "Friends on Both Sides of Film". http://www.caller2.com/2001/april/27/today/ricardob/24440.html. Retrieved 2001-04-27. from the Corpus-Christi Caller Times
- ↑ "'The Specials' internet documentary series". http://www.the-specials.com/home/.
- ↑ "Yo También on the Internet Movie Database". http://www.imdb.com/title/tt1289449/. Retrieved 2009-10-20.
- ↑ DSIAM — Down Syndrome in Arts & Media website. Retrieved 02-18-10.
- ↑ Online 'Mendelian Inheritance in Man' (OMIM) AMYLOID BETA A4 PRECURSOR PROTEIN; APP -104760, gene located at 21q21. Retrieved on 2006-12-05.
- ↑ Shekhar, Chandra (2006-07-06). "Down syndrome traced to one gene". The Scientist. http://www.the-scientist.com/news/display/23869/. Retrieved 2006-07-11.
- ↑ 101.0 101.1 Online 'Mendelian Inheritance in Man' (OMIM) V-ETS AVIAN ERYTHROBLASTOSIS VIRUS E26 ONCOGENE HOMOLOG 2; ETS2 -164740, located at 21 q22.3. Retrieved on 2006-12-05.
- ↑ Kuhn DE, Nuovo GJ, Terry AV Jr, Martin MM, Malana GE, Sansom SE, Pleister AP, Beck WD, Head E, Feldman DS, Elton TS. (2010). Chromosome 21-derived microRNAs provide an etiological basis for aberrant protein expression in human Down syndrome brains. J Biol Chem. 285(2):1529-43. doi:10.1074/jbc.M109.033407 PMID 19897480.
- ↑ Ellis JM, Tan HK, Gilbert RE (2008). "Supplementation with antioxidants and folinic acid for children with Down's syndrome: randomised controlled trial". BMJ 336 (7644): 594–7. doi:10.1136/bmj.39465.544028.AE. PMID 18296460.
References
Research bibliography
- Arron JR, Winslow MM, Polleri A (2006). "NFAT dysregulation by increased dosage of DSCR1 and DYRK1A on chromosome 21". Nature 441 (7093): 595–600. doi:10.1038/nature04678. PMID 16554754.
- Epstein CJ (June 2006). "Down's syndrome: critical genes in a critical region". Nature 441 (7093): 582–3. doi:10.1038/441582a. PMID 16738647.
- Ganong, W.J. (2005). Review of Medical Physiology (21st ed.). New York: Mc-Graw Hill. ISBN 0071402365.
- Nelson DL, Gibbs RA (2004). "Genetics. The critical region in trisomy 21". Science (journal) 306 (5696): 619–21. doi:10.1126/science.1105226. PMID 15499000.
- Olson LE, Richtsmeier JT, Leszl J, Reeves RH (2004). "A chromosome 21 critical region does not cause specific Down syndrome phenotypes". Science (journal) 306 (5696): 687–90. doi:10.1126/science.1098992. PMID 15499018.
- Hattori M, Fujiyama A, Taylor TD (2000). "The DNA sequence of human chromosome 21". Nature 405 (6784): 311–9. doi:10.1038/35012518. PMID 10830953.
- Underwood, J.C.E. (2004). General and Systematic Pathology (4th ed.). Edinburgh: Churchill Livingstone. ISBN 0443073341.
General bibliography
- Beck, M.N. (1999). Expecting Adam. New York: Berkley Books.
- Buckley, S. (2000). Living with Down Syndrome. Portsmouth, UK: The Down Syndrome Educational Trust. ISBN 1903806011. http://books.google.com/?id=__5wB08U2hMC.
- Down Syndrome Research Foundation (2005). Bright Beginnings: A Guide for New Parents. Buckinghamshire, UK: Down Syndrome Research Foundation. http://www.dsrf.co.uk/Reading_material/Bright_beginnings.htm.
- Dykens EM (2007). "Psychiatric and behavioral disorders in persons with Down syndrome". Ment Retard Dev Disabil Res Rev 13 (3): 272–8. doi:10.1002/mrdd.20159. PMID 17910080.
- Hassold, T.J., D. Patterson, eds. (1999). Down Syndrome: A Promising Future, Together. New York: Wiley Liss.
- Kingsley, J.; M. Levitz (1994). Count Us In: Growing up with Down Syndrome. San Diego: Harcourt Brace.
- Koch, Richard; De La Cruz, Felix F, eds (1975). Downs Syndrome...: Research, Prevention and Management. Proceedings of a Conference on Down's Syndrome. New York: Brunner/Mazel. ISBN 0-87630-093-X
- Pueschel, S.M., M. Sustrova, eds. (1997). Adolescents with Down Syndrome: Toward a More Fulfilling Life. Baltimore, MD: Paul H. Brookes.
- Selikowitz, M. (1997). Down Syndrome: The Facts (2nd ed.). Oxford, UK: Oxford University Press. ISBN 0192626620.
- Van Dyke, D.C.; P.J. Mattheis, S. Schoon Eberly, J. Williams (1995). Medical and Surgical Care for Children with Down Syndrome. Bethesda, MD: Woodbine House. ISBN 0933149549.
- Zuckoff, M. (2002). Choosing Naia: A Family's Journey. New York: Beacon Press. ISBN 0807028177.
External links
- Facts about Down Syndrome from the National Institutes of Health
- Tying Your Own Shoes An animated documentary that provides insight into the lives of four adult artists with Down Syndrome, by National Film Board of Canada
|
|||||||||||||||||||||||||||||||||||||